Clarify Health and Ideon Partner to Build Stronger, More Competitive Health Plan Networks
Clarify Health
JUNE 29, 2023
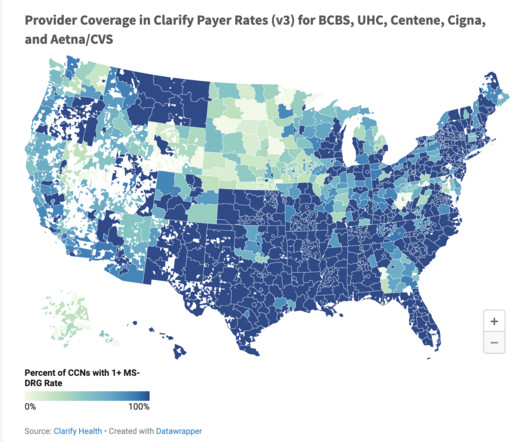
Clarify Health is leveraging Ideon, the industry’s most accurate and comprehensive provider-network data solution, to improve health plan management, lower costs and promote high-quality healthcare. Health plans can use this intelligence to expedite their decision-making processes for network modeling and optimization.
































Let's personalize your content