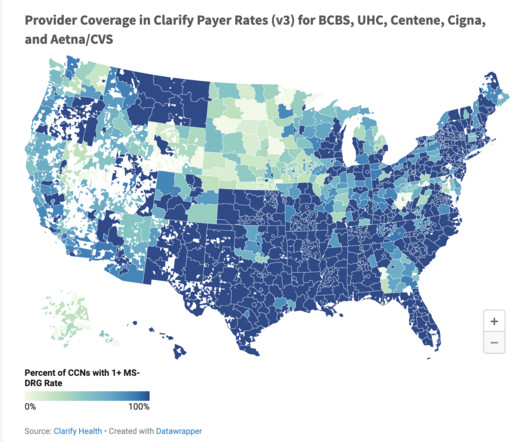
Three Strategies to Optimize Healthcare Provider Networks in New and Existing Markets
Clarify Health
SEPTEMBER 5, 2023
Optimizing provider networks is the number one way to do so. Provider networks are the primary tool for health plans to attract and retain new members while optimizing returns. This makes network design a key factor in any member retention strategy. to 30% of the time.





















Let's personalize your content