A Primer on Telepharmacy
Telepharmacy is growing at a rapid pace. Some of the country’s largest healthcare companies (e.g., CVS, Walgreens, and Optum) are using telepharmacy as part of their long-term strategy to deliver whole-person healthcare.
And that’s because pharmacy is an incredibly important part of the healthcare ecosystem—for many patients, they see their pharmacist far more often than their primary care physician.
Unfortunately, only about half of the states have adopted some form of telepharmacy (click here for an interactive map). Further, there exists little alignment among these states regarding the types of permissible telepharmacy services and the nature of a compliant telepharmacy operation.
For this reason, it’s important for innovators to understand relevant state law before embarking upon a telepharmacy program.
In this article, you will gain a high-level understanding of telepharmacy and how you can use and implement telepharmacy to positively impact patients, pharmacies, and healthcare providers.
The Evolution of Telepharmacy
Within the United States, telepharmacy emerged in the early 2000s in North Dakota as a way to address the lack of pharmacy access in rural areas of the state. North Dakota State University conducted a study in 2002, known as the North Dakota Telepharmacy Project, to evaluate the safety and efficacy of telepharmacy and found that it [telepharmacy] was as safe or safer than other forms of traditional pharmacy services.
Due to the success of the North Dakota Telepharmacy Project, the Board of Pharmacy in North Dakota permanently implemented telepharmacy regulations in 2003. Other states across central and western America, especially in rural communities, began to follow suit shortly thereafter, though national adoption still lags.
What is Telepharmacy?
Telepharmacy is used primarily to expand access to pharmacy services in rural or medically underserved areas.
According to the National Association of Boards of Pharmacy (“NABP”), telepharmacy means the “provision of pharmaceutical care through the use of telecommunications and information technologies to patients at a distance.”
What does that mean? Basically, it’s a method used in pharmacy practice in which a pharmacist utilizes remote communication technology (e.g., live video platforms) to oversee aspects of pharmacy operations or provide remote patient care services.
Telepharmacy is often confused with tele-prescribing/online prescribing and e-prescribing, so it’s worth defining the differences here.
Tele-prescribing/online prescribing definitions and rules vary by state, but the term generally refers to a clinician developing a relationship with a patient via telemedicine and then prescribing a drug to that patient. E-prescribing is the practice of electronically sending a prescription directly to a pharmacy from the point-of-care.
How Does Telepharmacy Work in Practice?
Because the practice is a relatively novel phenomenon, pharmacists and telepharmacy technology vendors are still developing creative ways to provide and facilitate these services, while still operating within the confines of the law.
Telepharmacy services generally fall within one or more of the following four categories:
Patient counseling. Patient counseling is one of the most valuable services that pharmacists can provide via telepharmacy technology. Virtual patient counseling enables patients to talk with their pharmacists more frequently and conveniently about questions they may have about their medication, which can ultimately help improve things like medication adherence.
Medication or disease management. Medication or disease management may include remote drug therapy monitoring, medication therapy management, or chronic care management, which can all be provided virtually via an integrated pharmacist-patient platform.
Medication review. Medication review includes medication reconciliation, which involves identifying and developing the most accurate list of all medications a patient is taking. This typically occurs in the inpatient setting. Medication review also includes new medication counseling, which may also occur in the inpatient setting upon patient discharge. Although hospitals have in-house pharmacists, they often experience staffing and time constraints. Offsite telepharmacy support can alleviate these challenges and help hospitals implement higher-quality medication reconciliation programs.
Remote verification. Remote verification typically involves a pharmacist remotely supervising a pharmacy technician as she prepares prescriptions for dispensing. This enables pharmacies to operate with more efficient staff structures, and for extended hours (e.g., after the pharmacist-in-charge on location leaves for the day).
Automated Dispensing Machines. Automated dispensing machines are digital drug storage, dispensing, and monitoring devices. Some healthcare settings, such as hospitals and nursing homes, use automatic dispensing machines to distribute medications safely in the absence of a licensed pharmacist.
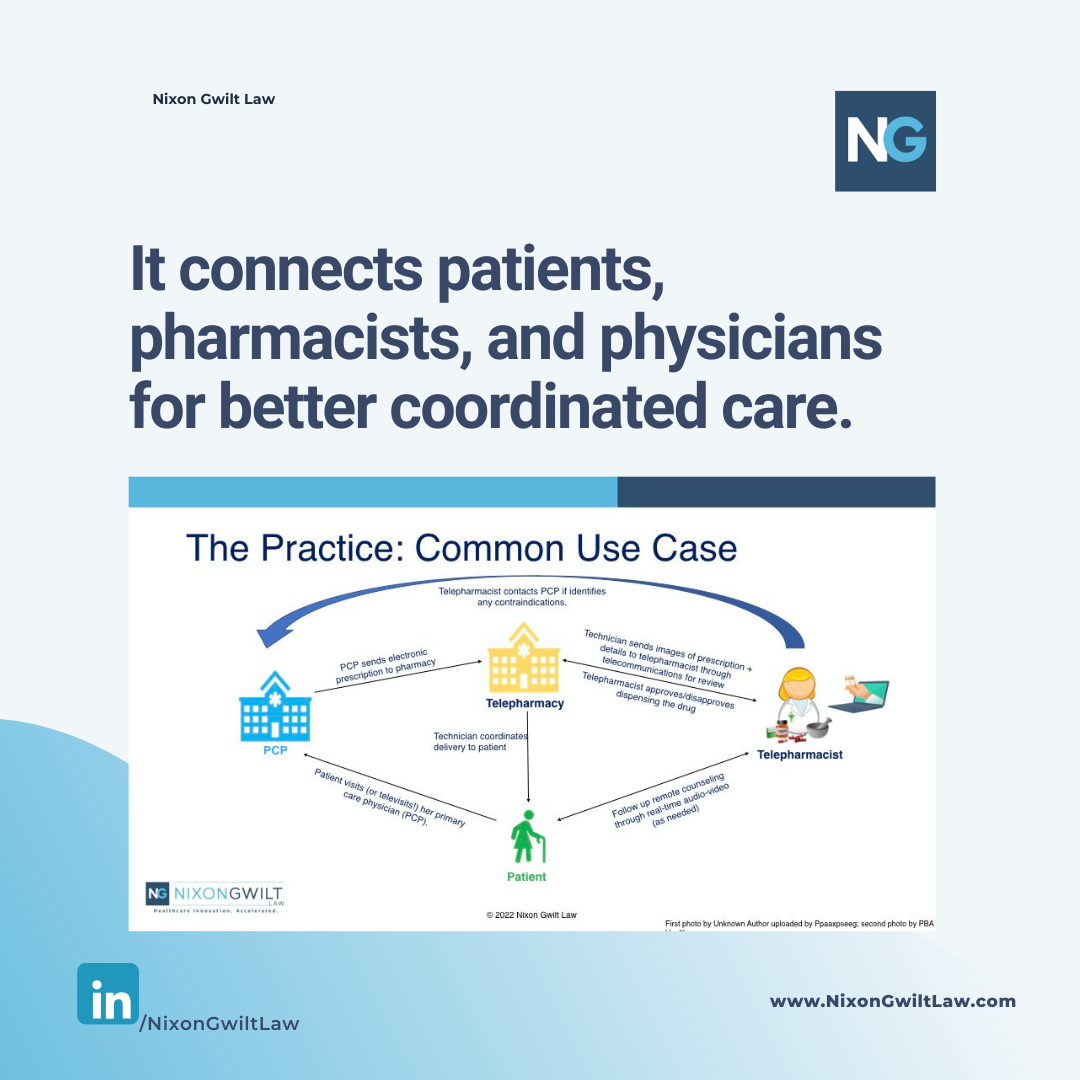
A common telepharmacy use case involves a primary care physician (“PCP”), a telepharmacy, and a tele-pharmacist who together coordinate patient care in the following manner:
Infographic created by Reema Taneja, Esq. and Rebecca Gwilt, Esq.
Telepharmacy Contributes to Better Care, Better Outcomes, and Healthy Equity
Because telepharmacy allows clinicians to provide patient counseling and other essential pharmacy services more effectively, with less friction, and close to the point of care, it has the potential to meaningfully improve patient care and outcomes. Telepharmacy can also reduce costs, particularly by facilitating increased access to medication management and medication adherence services, so it is ripe for use in value-based care.
In addition, like telehealth, telepharmacy can contribute to health equity. Often, patients of lower socioeconomic status are less able to physically visit their pharmacy due to transportation issues or the inability to take the time off from work. Telepharmacy may allow these patients to obtain services from wherever is most accessible for each patient. Telepharmacy is especially valuable in “pharmacy deserts” – areas where there are significantly few physical pharmacies.
Challenges to the Expansion of Telepharmacy
As stated above, only about half the states have passed legislation to allow “telepharmacy” in their pharmacy practice acts as a permissible form of pharmacy practice. Each state’s laws define the extent to which the practice is permitted.
For example, California permits the practice of telepharmacy but only in medically underserved areas unless otherwise approved by the Board of Pharmacy (Source: Cal. Bus. & Prof. Code § 4130).
Direct reimbursement is a barrier as well. Federal and most state* healthcare programs have yet to add specific telepharmacy services to their fee schedules, which hinders the pace at which telepharmacy can grow in a financially sustainable manner.
State Boards of Pharmacy are the entities overseeing the practice of telepharmacy, making recommendations, issuing guidance, and regulating what types of services can be provided and can therefore be instrumental in expanding access to these medically necessary services. Stakeholders interested in expanding telepharmacy should meet with their state Board of Pharmacy officials to push for the adoption of these services.
*North Dakota incorporated telepharmacy visits into its Medicaid manual. See Pharmacy Medical Billing Manual, North Dakota Department of Human Services, available at https://www.nd.gov/dhs/services/medicalserv/medicaid/docs/pharmacy-medical-billing-manual.pdf.
Telepharmacy is Gaining Momentum
As we saw during the COVID-19 public health emergency, patients across the country benefited from receiving prescription delivery and pharmacy services within the comfort of their own homes. In response, more and more pharmacies are starting to implement additional remote services like virtual patient consultations to assist patients, remote medication management, and connecting with providers to manage chronic disease.
Consumer demand for the convenience of virtual pharmacy services is likely to drive growth in the industry.
What’s Next?
There’s growing appetite and opportunity in the telepharmacy space, and it’s important for innovators in this space to structure their telepharmacy model in a compliant and scalable manner.
In future posts, we will cover federal and state laws related to telepharmacy and how to navigate these laws to build sustainable businesses.
Click here to get legal and business insights for innovative pharmacies delivered straight to your inbox.