The adoption of Electronic Health Records (EHRs) had been a slow process until 2009 when federal incentives to healthcare professionals (HCPs) to switch from paper to EHR charts became available, and when HCPs were rewarded via higher payments for meeting meaningful use criteria. HCPs needed to show they could utilize a certified EHR in a meaningful way (i.e., make patient’s health information available online within a short period of time, facilitate the electronic exchange of health information to improve the quality of care delivered, and submit clinical quality data to reimbursement authorities as required).
Fast forward to today when more than 90% of HCPs are on an EHR, and more than five hours of an eight-hour day are spent in the EHR.1 EHRs have become the primary means for registering and seeing patients, making and documenting diagnoses, prescribing treatments, and implementing follow up, all in the pursuit of improving outcomes (both clinical and economic) and the user experience in healthcare. In addition, EHRs can track specific outcomes in support of value-based payments as well as help reduce medical errors (e.g., by flagging potential drug-drug interactions at the point of prescribing).
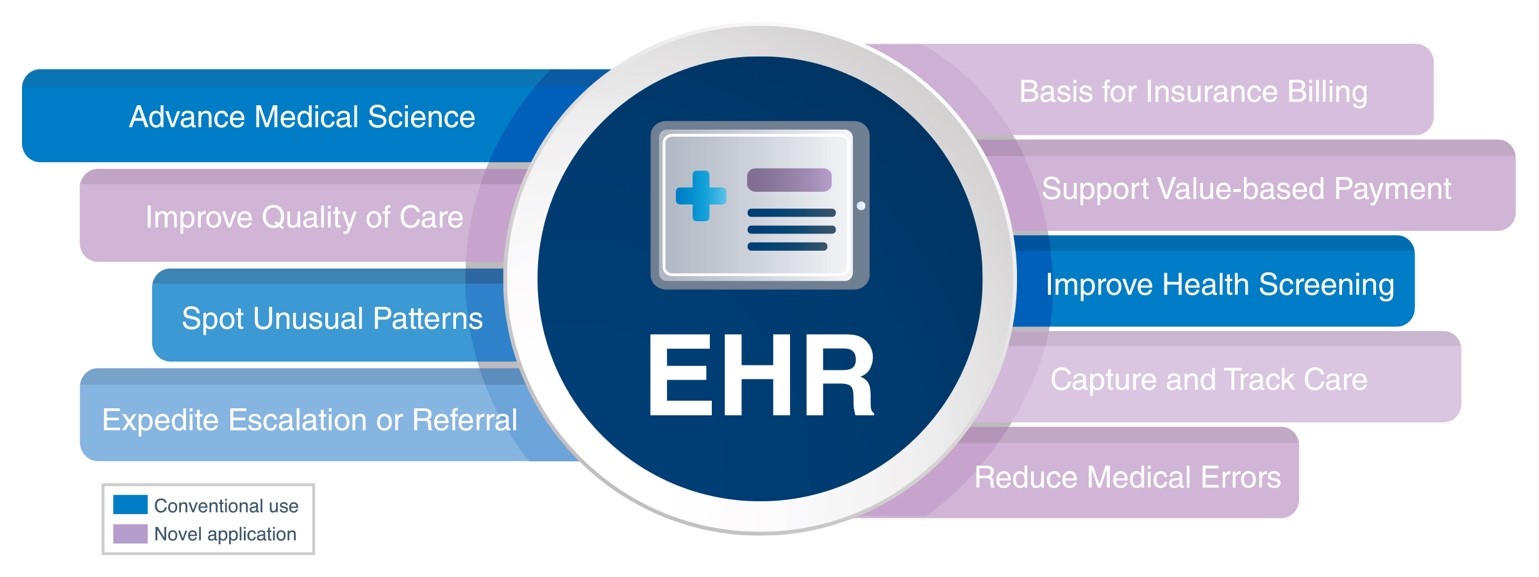 In parallel, life sciences companies have become increasingly aware of the ability to harness EHR data to solve for numerous challenges both in the pre-approval and post-commercialization arenas. Here are four examples of innovative applications that are gaining traction.
In parallel, life sciences companies have become increasingly aware of the ability to harness EHR data to solve for numerous challenges both in the pre-approval and post-commercialization arenas. Here are four examples of innovative applications that are gaining traction.
1. Improve Health Screening
EHRs have a critical role to play in improving health screening that, in turn, advances health. Two examples capture the EHR’s potential. First, finding patients missing a specific immunization. The COVID pandemic brought to light the need to closely monitor vaccination rates, and most importantly, vaccination gaps for the multitude of immunizations that are recommended from the HPV vaccine in teenagers to the shingles vaccine in adults over 55.
Case in point, the CDC’s Advisory Committee on Immunization Practices (ACIP) released new pneumococcal vaccine recommendations this year.2 The recommendations are based on age, underlying medical conditions, and pneumococcal immunization history. Each of these variables is available as structured data in an EHR. Using the patient list functionality to find patients who meet each of the scenarios defined in the ACIP recommendations gives a practice or health system top line metrics on vaccination gaps—and directs their efforts to those patients who are eligible for additional vaccination. Closing these gaps in pneumococcal immunization has direct clinical and economic benefits in reducing sequalae associated with pneumococcal disease.
Second, EHRs can help find patients who are missing or overdue a crucial lab test. In today’s quality-driven environment, HCPs and population health managers are focused on achieving specific quality metrics to provide evidence-based medicine as well as receive incentive payments associated with achieving them. As an example, a new NCQA HEDIS quality measure looking at the percentage of patients with type 2 diabetes (T2D) who had a kidney health evaluation in the last year was rolled out in 2020. The measure is seeking to improve the percentage of adults with T2D who received an annual kidney health evaluation, which includes both an estimated glomerular filtration rate (eGFR) and a urine albumin-creatinine ratio (uACR).3
EHR patient lists can readily identify the patients who do not have both kidney measures, estimated to be about half of all adults with T2D. Once run, the missing tests can be ordered, patients can be communicated to, and downstream, more patients who have kidney disease can be diagnosed and treated. The potential for this EHR capability to support HCPs in identifying eligible patients who may be appropriate for drugs that have been shown to help preserve renal function in diabetics is obvious, as are many other examples.
2. Support “Watchful Waiting”
In many medical conditions time is a critical factor in securing appropriate care and improving outcomes. An EHR has the potential to support an HCP in “watchful waiting,” that is, tracking progress over time to help identify the “tipping point” at which further intervention is required, be it referral onward to a specialist or treatment escalation. For example, the cancer patient who initially responds well to first-line treatment but in whom the response declines over time. The EHR can be set to flag key indicators of treatment response and trigger further HCP action.
3. Spot Unusual Patterns
One huge benefit of having virtually all HCP/patient engagements in a digital format is the ability to use the EHR to query for specific variables that are captured in those encounters. Every EHR system can run queries for patients who meet specific clinical and/or demographic criteria. These queries can be run using standard reporting functionality (e.g., Epic Workbench), requiring minimal access rights from an end user, or more sophisticated SQL statements run against larger databases with less data restrictions (e.g., Epic Clarity).
One recent application was in helping to find patients with an unusual presentation of signs and symptoms who also received tests and treatments for minor illnesses affecting a variety of organ systems. While no one event would have been enough to trigger consideration of the syndrome under study, when combined with an EHR query the HCP was able to find and more formally assess patients with a confusing array of health issues.
4. Advance Medical Science
An EHR can help assess the viability of a planned clinical trial by finding patients who may be suitable for enrollment. The longer a trial takes to enroll patients, the smaller the return-on-investment that can be garnered post-approval. Today’s clinical research coordinators (CRC) and site nurses are both overworked and understaffed—and COVID has only exacerbated this challenge. Additionally, the same site often has competing studies for the same or similar indication. Therefore, the need to efficiently identify patients who meet most of the inclusion and exclusion criteria for a study, in a manner that doesn’t require a ton of additional work from the site, is a welcomed solution.
EHR patient lists can accomplish this through a step-by-step set of instructions to query the EHR with the inclusion/exclusion variables that are available via structured data format. These may be ICD10 or CPT codes, specific lab values, demographic variables, etc. Once run, the output will be a smaller group of patients with a higher probability of meeting the study criteria. This list can then be evaluated by the CRCs and site nurses for possible enrollment. Additionally, standard EHR functionality to communicate with patients (email, text, patient portal) can then be efficiently utilized as the sites seeks to enroll.
Summary
EHRs are much, much more than just a digital record of patient care. The original intended application of the EHR has, by-and-large, been successful. The exciting discussion is how the EHR/HIT infrastructure can be used in a legal and compliant manner to further advance patient care and population health. Note that in each example, the EHR application is entirely and without interruption in the hands of the licensed and credentialed HCP at the clinic or hospital, and the EHR data are never in the hands of any third-party sponsor such as a biotech or pharma manufacturer. The EHR patient list capability may be funded by a third-party but the use in patient-level data is not.
As we have highlighted, EHR patient lists can help the HCP solve for the problems of finding the right patients for clinical trials, further testing/assessment/evaluation, patients missing specific labs or vaccinations or other follow ups, and to support watchful waiting. Life sciences companies have evolved during the last two decades to better understand the business challenges their customers are faced within the EHR/HIT environment. Those companies that continue to seek out opportunities to assist their HCP customers in providing better care and a better user experience, using the multitude of EHR functions that are available, will continue to generate wins with HCPs, patients, and their brands.
References:
1. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2784810.
2. https://www.cdc.gov/mmwr/volumes/71/wr/mm7104a1.htm?s_cid=mm7104a1_w.









